Thyroid Nodule Biopsy: Cancer of Thyroid Nodules is Diagnosed by Fine Needle Aspiration Biopsy (FNA)
- FNA is an abbreviation for Fine Needle Aspiration Biopsy. This is a common test performed thousands of times per day on people with thyroid nodules.
- FNA is a type of biopsy. A biopsy is the removal of some cells from the body so they can be looked at under a microscope to see if the cells are cancerous.
- The only purpose of a FNA biopsy is to get cells from the thyroid (or lymph node) to look at under a microscope. If not enough cells are removed, the test is worthless or not diagnostic (discussed below).
- Thus, FNA is used to diagnose thyroid cancer in a patient with a thyroid nodule that is suspicious for cancer (most thyroid nodules are not cancerous).
- FNA biopsy can also be done on lymph nodes in the neck which are around the thyroid to see if there are any thyroid cancer cells inside the lymph nodes.
- Ultrasound allows the doctors to see the thyroid nodule or lymph node(s) during the needle biopsy, which helps make sure they are getting the needle stuck into the right areas.
- FNA biopsy is the same as: needle biopsy of thyroid, FNA needle biopsy, FNA of thyroid, etc. They are all the same thing so don't be confused.
- FNA needle biopsy of thyroid nodules is generally done on any thyroid nodules that is big enough to be felt. This means that they are larger than about 1 centimeter (about 1/2 inch) across.
- FNA biopsy is indicated on any thyroid nodule that causes symptoms. We have an entire page on symptoms caused by thyroid nodules.
- FNA biopsies should be done on any swollen or abnormal lymph nodes in the neck. This may be more accurate in diagnosing thyroid cancer than FNA of the thyroid nodule itself!
- FNA biopsy should be done on thyroid nodules that have a certain characteristic under the ultrasound.
-
The process of obtaining this small sampling of cells is called fine needle aspiration (FNA) cytology or FNA biopsy.
- FNA needle biopsy can usually be done in your doctor’s office or clinic. Almost always by an endocrinologist or a radiologist with expertise in FNA biopsy.
- Before the FNA biopsy, local anesthesia (numbing medicine) is injected into the skin over the thyroid nodule.
- Ultrasound will be used so the doctor can see the nodule (or lymph node). They can see the needle going into the nodule.
- Your doctor will place a thin, hollow needle directly into the nodule to aspirate (take out) some cells and possibly a few drops of fluid into a syringe.
- The doctor usually repeats this 2 or 3 more times, taking samples from several areas of the nodule.
- The content of the needle and syringe are then placed on a glass slide and then the FNA samples are then sent to a lab, where they are looked at under a microscope by the expert Cytologist to see if the cells look cancerous or benign.
- Cytology means looking at just the cells under the microscope.
- Thyroid cytology requires an expert physician (called a Cytologist) trained specifically in the diagnosis of thyroid nodules and thyroid cancers!
- The FNA needle biopsy is only as good as the guy holding the needle. Experience counts!
- The diagnosis of thyroid cancer by FNA biopsy are frequently misinterpreted by unskilled or inexperienced Cytologists. The guy looking into the microscope needs to be experience too because they can get it wrong!
- Bleeding at the FNA biopsy site is very rare except in people with bleeding disorders. Even when this occurs, the bleeding is almost always very self limited. Be sure to tell your doctor if you have problems with bleeding or are taking medicines that could affect bleeding, such as aspirin or blood thinners.
- Sometimes an FNA biopsy will need to be repeated because the samples didn’t contain enough cells. This is called an "inadequate specimen", meaning the needle didn't suck up enough cells for the cytologist to look at under the microscope.
- Most FNA thyroid biopsies will show that the thyroid nodule is benign, because, most thyroid nodules are benign (non-cancerous).
- Rarely, the FNA thyroid biopsy may come back as benign even though a diagnosis of a thyroid cancer is actually present. In other words, it is possible (but quite rare) for the nodule to be cancerous but the result of the cytology report is that no cancer is present (benign).
- Sometimes the cytology (microscope) results of the FNA biopsy comes back as “suspicious” for a diagnosis of papillary thyroid cancer. When this happens, the decisions made should be just like the diagnosis of papillary thyroid cancer is made. In other words, if the FNA results say "suspicious for cancer" then we treat it like it is cancer. Suspicious for cancer is treated the same as if it was diagnosed as cancer.
- The Veracyte / Afirma test has the best ability to tell whether the FNA cytology is benign. This is called a “rule out” test. It is really good at seeing if a thyroid nodule is benign. If this test tells you the needle biopsy is benign, then the possibility of it actually being a cancer is less than 4%.
- Both Asuragen and Thyroseq are “rule in” tests. This means that they look for genetic abnormalities known to be associated with a diagnosis of thyroid cancers. Finding these particular genetic changes makes a diagnosis of thyroid cancer much more likely, and in some circumstances may also play a role in determining the best surgery for the cancer.
- Thyroid Nodule Overview. The basics of thyroid nodules, what they are and who gets them.
- Symptoms of Thyroid Nodules. Most nodules don't cause symptoms, but if they do surgery is needed.
- Thyroid Nodule Treatment Learn all options for thyroid nodules, including doing nothing!
- Overview of Thyroid Cancer.This is where you start this site to learn about thyroid cancer.
- How to Become Our Patient and have the best thyroid cancer team in the world take care of you.
Who needs a FNA needle biopsy of their thyroid nodule?
Thyroid nodules are common, with most people over the age of 50 having at least one thyroid nodule. The incidence of thyroid nodules is your age + 10. Thus, about 60% of people 50 years of age have a thyroid nodule, and 80% of people who are 70 years old will have a thyroid nodule. Obviously we aren't sticking needles (FNA biopsies) in everybody... So who needs to have their thyroid nodule biopsied? The answer is that FNA biopsy should be done on any nodule that the doctor thinks may be cancerous. There are certain characteristics of thyroid nodules that make doctors concerned; here is a list of them:
How is a FNA Needle Biopsy of the Thyroid Done?
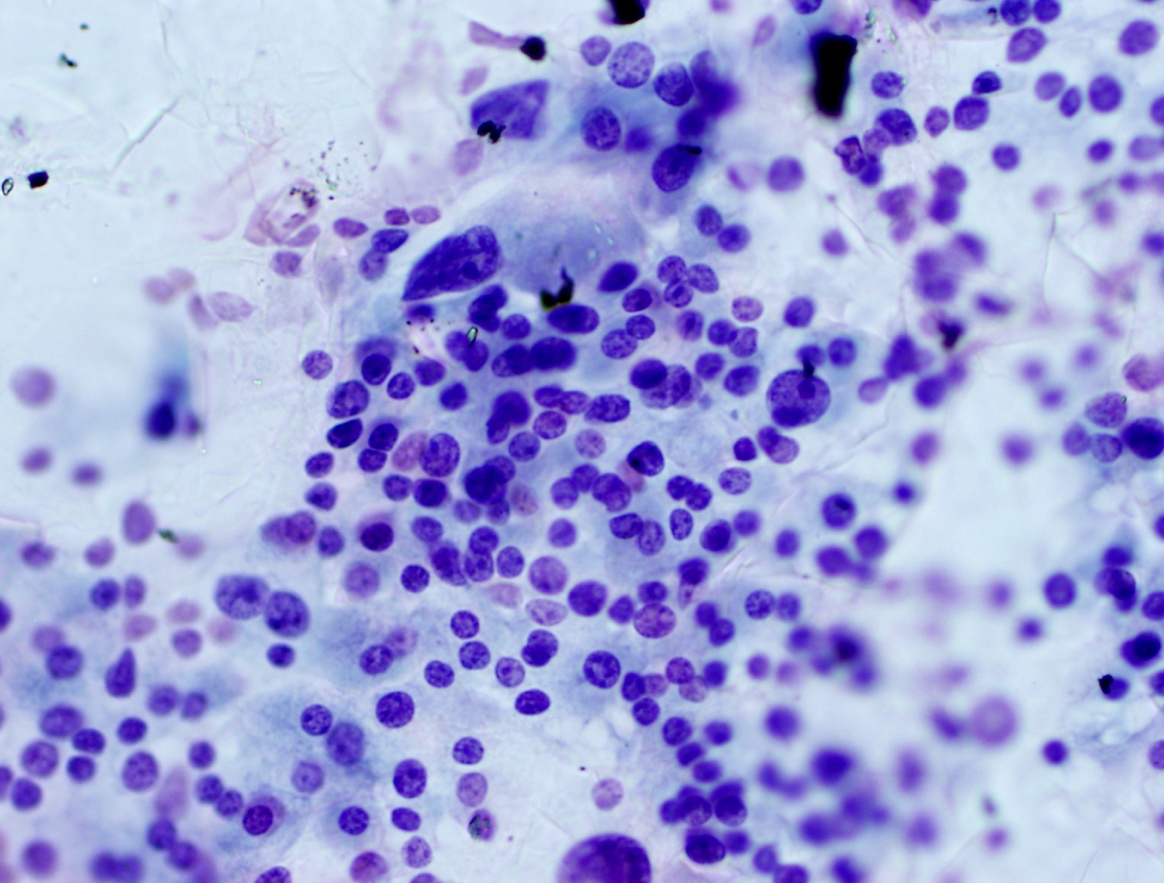 This picture shows a cytology slide of an FNA needle biopsy of a thyroid nodule. When the doctor sticks the needle into the nodule he/she sucks (aspirates) cells up the needle into a small syringe. They then squirt the content of the syringe onto a glass microscope slide which then has some special dyes put on it to color different parts of the cells. This slide shows lots of cells and is a very good slide. If only a few cells were on the slide, the cytologist would say it was "inadequate" and thus worthless to say anything about thyroid cancer yes/no. They can't tell if it's cancer if they don't have enough cells. The cytologist looks at the size and shape of the cells. They look at the dark material in the center of the cell--this is the DNA within the nucleus or center of the thyroid cell. In this slide you can see some of the cells are bigger and the nucleus appears to be “clearing” compared to other cells. This clearing of the nucleus means this FNA biopsy is suspicious for a diagnosis of papillary thyroid cancer.
This picture shows a cytology slide of an FNA needle biopsy of a thyroid nodule. When the doctor sticks the needle into the nodule he/she sucks (aspirates) cells up the needle into a small syringe. They then squirt the content of the syringe onto a glass microscope slide which then has some special dyes put on it to color different parts of the cells. This slide shows lots of cells and is a very good slide. If only a few cells were on the slide, the cytologist would say it was "inadequate" and thus worthless to say anything about thyroid cancer yes/no. They can't tell if it's cancer if they don't have enough cells. The cytologist looks at the size and shape of the cells. They look at the dark material in the center of the cell--this is the DNA within the nucleus or center of the thyroid cell. In this slide you can see some of the cells are bigger and the nucleus appears to be “clearing” compared to other cells. This clearing of the nucleus means this FNA biopsy is suspicious for a diagnosis of papillary thyroid cancer.
Does FNA biopsy always work? Does FNA needle biopsy of the thyroid always tell cancer of the thyroid?
FNA needle biopsy of thyroid nodules is a very reliable test that works great in most cases. Unfortunately, FNA needle biopsy of the thyroid doesn't always work and in about 25% of cases the biopsy is not good and nothing can be determined. In other words, in about 25% of cases, the FNA biopsy is worthless. It is very important for you to know that a doctor who performs FNA all the time (an expert in thyroid biopsy who does 5 or more per week) has a much higher success rate, with less than 10% of cases being "inadequate" (a nice word for useless!). Doctors who perform FNA biopsy only occasionally will have biopsies that are inadequate or indeterminant much more often, even as high as 40% of these biopsies having no useful data. It is very important for you to chose the most experienced doctor you can. Find an expert so you don't waste your time and you get the most accurate information! Here are some facts about FNA needle biopsy of the thyroid:
Indeterminant Thyroid Nodule Biopsy: What happens if the biopsy has a result of "Undetermined Significance (ACUS)?
ACUS is an abbreviation for “atypical cells of undetermined significance”. This occurs when the thyroid FNA findings don’t show for sure if the nodule is either benign or malignant. The pathologist looks at the cells and just can't be sure if it is cancer, or non-cancer (benign). If this happens, an option that your doctor has is to genetic testing done on the cells of the biopsy to see if there are genetic abnormalities seen. There are several commercially available tests that doctors can send the samples to determine the risk of the cells being cancerous--they look for several specific abnormal pieces of DNA that are frequently associated with thyroid cancer. Before you consider one of these genetic tests, you should ask yourself “what information do I seek?” and “How will this information change my approach to my thyroid mass?” The point being, many thyroid nodule biopsies do not need this expensive genetic testing , and if the answer isn't going to change what you are going to do, then don't spend the extra money (and time) getting genetic testing. For example, if the thyroid nodule has other characteristics or symptoms and the plan is to have surgery to remove the nodule, then don't bother with the genetic testing. It won't change what you are planning on doing--you are already planning surgery.
Sometimes the genetic testing will indicate surgery is necessary. For example, if you have a small thyroid nodule that is less than 1.5 cm and the FNA biopsy result is "atypical cell of undetermined significance" (ACUS) and the plan was to just monitor the nodule with ultrasound every year, then getting genetic testing could change this plan and lead you to a surgery if the nodule contains a specific abnormal gene that is associated with thyroid cancer. In this case, the genetic testing changed the plan from "monitoring" to surgery.
From an opposite standpoint, if you are above 5o years of age and have a 4cm thyroid nodule that has abnormal vascularity and the FNA biopsy of the nodule is "atypical cells of undetermined significance" (ACUS) then genetic testing may not be necessary because surgery would already be recommended for multiple reasons including ultrasound appearance, the large size of the nodule, and your age. Genetic testing of this thyroid nodule would only be beneficial in this circumstance if the surgeon and patient would propose a total thyroidectomy based upon this additional information (instead of just a thyroid lobectomy).
Genetic Testing of Thyroid Nodules: Veracyte / Afirma, Asuragen, and Thyroseq
There are three commercially available genetic testing companies for thyroid nodules: Veracyte (Afirma), Asuragen, and Thyroseq. They are similar, but each has some unique advantages. Typically your doctor will send your FNA biopsy specimen to just one of these three. Here are some specifics about the genetic thyroid tests:
If your FNA biopsy doesn't give you a good, reliable answer, (if it cannot tell the difference between a benign thyroid nodule and a thyroid cancer), you might need to take more invasive steps and even a biopsy during surgery to get a better sampling of cells from the thyroid nodule so the pathologist has more cells to examine under the microscope. If the doctor has reason to think the nodule is suspicious or worrisome for a thyroid cancer based upon the nodule size, symptoms, or ultrasound appearance, the preferred biopsy is to not stick needles in it again, but instead to REMOVE that entire half of the thyroid (called a thyroid lobectomy). The entire thyroid nodule will come out with the half of the thyroid (the thyroid "lobe") that it is growing in. A thyroid lobectomy can also be the main treatment for many patients with a diagnosis of thyroid nodules as well as many thyroid cancers. Said differently, sometimes removing half of the thyroid (thyroid lobectomy) will be all the surgery a patient needs and the cancer can be cured during this one operation. We have several videos discussing the pros and cons of removing half of the thyroid for thyroid cancer. There are many patients that can be cured of thyroid cancer just by removing half of the thyroid.